This article presents a clinical case of a patient X suffering for a long time from coronary artery disease causing considerable myocardial ischemia accompanied by attacks of paroxysmal supraventricular tachycardia (TPSV). In this clinical case, the results of the Cardioversion performed on patient X are described during one of these attacks of TPSV with arrhythmic shock in conditions of emergency medical intervention at home -SAMU. The purpose of the examination of this clinical case — to draw special attention to this category of patients from the doctors and paramedics of the ERM, cardiologists, anesthesiologists, reanimatologists and therapists to be able to consider cardioversion as soon as possible as therapy in the face of a similar case.
Keywords: coronary artery disease, supraventricular paroxysmal tachycardia, cardioversion, arrhythmic shock, deep sedation.
In the Russian Federation at the moment although the treatment and preventive measures implemented by the Russian Ministry of Health, cardiovascular diseases as a pathology occupies the first place in the structure of morbidity and mortality. According to Rosstat, starting from 2010, a reduction in mortality from cardiovascular causes or accidents is regularly observed. However, cardiovascular diseases (CVD) remain the main cause of death of Russians (47 %). The first place in the structure of causes of death from CVD is occupied by coronary heart disease. The annual number of deaths from coronary heart disease among the population in Russia — 27 % [1]. CVD is the main cause of heart rhythm disturbances, leading to the appearance of attacks of various types of arrhythmia, which can be complicated by arrhythmic shocks and cases of sudden death.
Myocardial ischemia — this is a defect of insufficiency in the blood supply of the myocardium, caused by a violation of blood circulation by the coronary arteries -coronary heart disease [3]. Myocardial ischemia occurs on functional and
organic, changes in the myocardium. Atherosclerosis of the coronary arteries is the leading cause of organic myocardial damage. It is equipped with a change including arterial thrombosis, heart rhythm disturbances (arrhythmia). Myocardial ischemia includes unstable acute and stable chronic conditions. Among the acute unstable states of this pathology, the development of paroxysmal supraventricular tachycardia is one of the most frequently encountered.
Paroxysmal supraventricular tachycardia is one of the types of paroxysmal arrhythmia, which manifests itself in the form of heart attacks with a heart rate of 140–220 and more beats/min [4]. It develops under the ectopic influence of impulses in the ventricles, causing the replacement of the normal sinus rhythm. The heart attack is usually transient and stops by itself sometimes lasting from a few minutes to several days. Patients suffering from this pathology with arrhythmia take antiarrhythmic therapy, sometimes, need emergency provision in case of a paroxysmal supraventricular tachycardia heart attack, which can be complicated by ischemic shock. Infusion therapy- amiodarone 300 mg with glucose 5 %-250ml is not always effective in such cases. In this regard, the holding of cardioversion therapy remains the only choice of treatments.
Arrhythmic shock often occurs when paroxysmal supraventricular tachycardia, but it develops in the first hours of the disease and is accompanied by a critical condition of the patient significant manifestation of all clinical signs of cardial shock (severe hypotension, olygoanuria, symptoms of peripheral circulation insufficiency) [2]. In most cases the patients had a development of left ventricular failure, accompanied by pulmonary edema, cardiac asthma, ventricular fibrillation, thromboembolism of vital organs, [5].
Clinical case: Patient X, 56 years old suffering from coronary artery disease, Arterial hypertension stage-2, phase-2, risk-1, regularly receives antihypertensive drugs: Losartan, metoprolol, atorvastatin, cardiomagnile. 27.04.2024 contacted the emergency department of the SAMU at 103 complaining of general weakness, increased heart rate, dizziness, drop in blood pressure to 80/50 mm Hg and shortness of breath. According to the patient, these symptoms have been bothering since 8:05. Before the arrival of the brigade of the 2nd station of the Simferopol SAMU, the patient took a metoprolol tablet with no positive effect, the patient has a history of myocardial infarction on 06.01.2023, On arrival of the SAMU brigade, the general condition of the patient was assessed critically, the pale skin moist. Skin rashes, anysocorea, nystagmus, wheezing, signs of peritoneal irritation, vomiting and edema not recorded. Calm behavior, clear consciousness the Glasgow score: 15 (E 4 V 5 M 6), normal pupils, reactive to light, normal muscle tone, meningitis signs are negative, vesicular breathing strengthened, inspiratory shortness of breath, percussive lung clear sound. The heart sounds are clear rhythmic, pulse spinning arrhythmic, the tongue moist clean, the abdomen is supple and painless on palpation, participates in the act of breathing, active peristalsis, the liver is not increased. Urine and feces in the presence of the SAMU not visualizable.
For more than one set of objective data: the patient's actual weight of 87 kg, symmetrical face, tongue on the midline, speech and swallowing are not broken, symptoms of paresis and paralysis not recorded, muscle strength and limb sensitivity recorded, digitigrade and oleopneumatic presses heel spur tests performed with difficulty, but without deviations on both sides, in the romberg posture the patient is not resistant. The patient is oriented in space, time and personality.
Arterial blood pressure BP- 60/30 mm Hg, pulse 175 beats/min, heart rate 175 beats/min, breathing rate 25 beats/min, 94 % CO2, t 35.8 and Glucose 4.6 mmol/l. image1
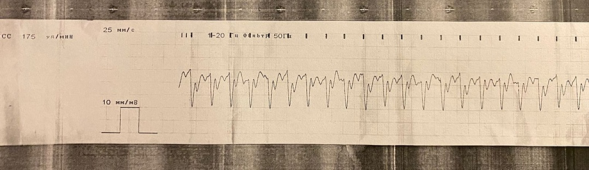
Fig. 1. L'ECG n ° 1
The ECG n ° 1: the non-sinus rhythm, regular, the ST segment on the isoline, the QRS complex enlarged and strongly deformed, the heart rate 175 beats/min, paroxysmal supraventricular tachycardia.
Diagnosis: Myocardial ischemia, paroxysmal supraventricular tachycardia (TPSV), post-infarction cardiosclerosis (2023). the state of arrhythmic cardiogenic shock.
Assistance in emergency medical care on site:
- The inspection of the patient. 09:57
- Functional state of the machine.
- The catheterization of the left and right ulnar veins.
- The inhalation of oxygen via the medical device through the face mask with the speed of 6 l/min
- The purpose of performing cardioversion, administration by venous routes: At 10:00
- Ground. Sibasoni 5mg/ml-2ml/in in IV.
- Phentanyli 50 mg/ml-2ml+ Sol. Natrii chloridi 0.9 %-10ml in IV.
Deep sedation began 10 minutes after the introduction of the sol. Sibasoni. Unstable hemodynamics: Arterial blood pressure BP- 60/30 mm Hg. The heart rate 166, the Pulse 175, S 12 94, t 35.8, respiratory rate 19 mt/min.
At 10:13 The 1st synchronized cardioversion took place the Minolvay defibrillator 1 time a series of electric energy — 150 J, the non-sinus rhythm, regular, the ST segment on the isoline, the QRS complex enlarged and strongly deformed, paroxysmal supraventricular tachycardia, the heart rate 166, BP- 60/30 mm Hg, the Pulse 175, the A2 97 %, respiratory rate 19 mt/min, t 35, 8. Sedation.
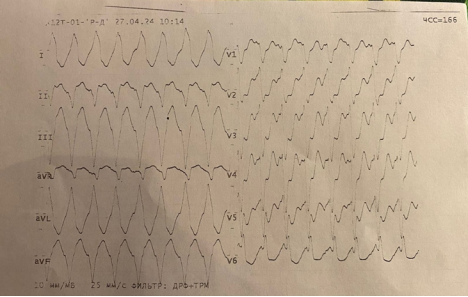
Fig. 2. L'ECG n ° 2
The ECG n ° 2: the non-sinus rhythm, regular, the ST segment on the isoline, the QRS complex enlarged and strongly deformed, paroxysmal supraventricular tachycardia, the heart rate 166 beats/min.
At 10:16, Second synchronized cardioversion the Minolvay defibrillator 1 time a 1 time a series of electric energy- 200 J. The recovery of the heart rate: the sinus rhythm, regular, the ST segment on the isoline, the deformed non-enlarged QRS complex, the heart rate 66 beats/min, BP- 80/50 mm Hg, the Pulse 66, 1.2 98 %, respiratory rate 18 mt/min, t 35, 8. Sedation.
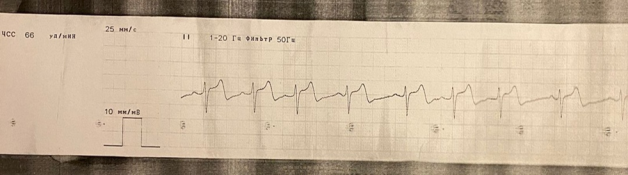
Fig. 3. L'ECG n ° 3
The ECG n ° 3: the sinus rhythm, regular, the ST segment on the isoline, the deformed non-enlarged QRS complex, the heart rate 66 beats/min, BP- 80/50 mm Hg, the Pulse 66, t 12 98 %, respiratory rate 18 mt/min, t 35, 8. Sedation.
Due to the hemodynamic instability of BP- 80/50 mm Hg, the patient is given an infusion: 10:18
Sol. Dopamine de 5 % 5ml+ Sol. Glucosae 5 %-250 ml.
Follow-Up:
10:18 — the sinus rhythm, regular, the ST segment on the isoline, the deformed non-enlarged QRS complex, the heart rate 66 beats/min, BP- 80/50 mm Hg, the Pulse 66, t 12 98 %, respiratory rate 18 mt/min, t 35, 8. Sedation.
10:23 — the sinus rhythm, regular, the ST segment on the isoline, the deformed non-enlarged QRS complex, the heart rate 66 beats/min, BP- 85/55 mm Hg, the Pulse 66, t 12 98 %, respiratory rate 18 mt/min, t 35, 8. Sedation.
10:28 — the sinus rhythm, regular, the ST segment on the isoline, the deformed non-enlarged QRS complex, the heart rate 66 beats/min, BP- 90/65 mm Hg, the Pulse 66, t 12 98 %, respiratory rate 18 mt/min, t 35, 8. Sedation.
10:33 — the sinus rhythm, regular, the ST segment on the isoline, the deformed non-enlarged QRS complex, the heart rate 66 beats/min, BP- 95/70 mm Hg, the Pulse 66, t 12 98 %, respiratory rate 18 mt/min, t 35, 8. The clear conscience on the Glasgow scale: 15(E 4 V 5 M 6).
10:38 — the sinus rhythm, regular, the ST segment on the isoline, the deformed non-enlarged QRS complex, the heart rate 66 beats/min, BP- 100/70 mm Hg, the Pulse 66, HR 12 98 %, respiratory rate 16 mt/min, t 36.3. The clear conscience on the Glasgow scale: 15(E 4 V 5 M 6).
10:43 — the sinus rhythm, regular, the ST segment on the isoline, the deformed non-enlarged QRS complex, the heart rate 66 beats/min, BP- 105/75 mm Hg, the Pulse 66, t 12 98 %, respiratory rate 16 mt/min, t 36, 3. The clear conscience on the Glasgow scale: 15(E 4 V 5 M 6).
10:48 -the sinus rhythm, regular, the ST segment on the isoline, the deformed non-enlarged QRS complex, the heart rate 66 beats/min, BP — 110/75 mm Hg, the Pulse 66, t 12 98 %, respiratory rate 16 mt/min, t 36, 3. The clear conscience on the Glasgow scale: 15(E 4 V 5 M 6).
10:53 was removed from ECG control.
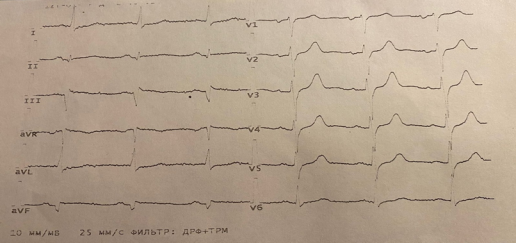
Fig. 4. L'ECG n ° 4
The ECG n ° 4: the sinus rhythm, regular, the ST segment on the isoline, the QRS complex not enlarged deformed, the heart rate 66 beats / min.
BP- 120/80 mm Hg, Pulse 66, CO2 concentration 99 %, respiratory rate 16 mt/min, t 36, 3. The clear conscience on the Glasgow scale: 15(E 4 V 5 M 6).
BP- 120/80 mm Hg. The heart rate is 65, the Pulse is 65, SrO2 is 98 %, respiratory rate 16 mt/min, t 36, 3.
The general condition of the patient is stable, the consciousness is clear on the Glasgow scale: 15(E 4 V 5 M 6).
Conclusion
Therefore, to this clinical case presented the results and the effectiveness of conducting cardioversion therapy on patient X presenting a paroxysmal attack of supraventricular tachycardia with arrhythmic cardiogenic shock. According to the results of carrying out cardioversion emphasizes the re-initialization of the sinus rhythm of the heart rate and Hemodynamic parameters after cardioversion and intensive and complex therapy. The patient's vital signs are stable: BP- 120/80 mm Hg, Pulse 66, pH 12 99 %, respiratory rate 16 mt/min, t 36, 3. The clear conscience on the Glasgow scale: 15(E 4 V 5 M 6). As a result, it should be noted that, cardioversion was successfully performed, the paroxysmal supraventricular tachycardia attack with arrhythmic cardiogenic shock cropped.
References:
- Ventricular rhythm disturbances. Ventricular tachycardia and sudden cardiac death. Medelement [electronic Resource]. — URL: https://diseases.medelement.com.
- The state of cardiogenic shock (R57.0). Medelement [electronic Resource]. — URL: https://diseases.medelement.com.
- From the clinical recommendations «Stable coronary heart disease» (utv. The Ministry of Health of the RUSSIAN Federation, by 2020,)//national institute of clinical recommendations from 07.08.2020 g.
- Paroxysmal tachycardia. FGAOU DANS RNIMU leur. N. Vi Pirogov from The Ministry of Health of Russia. [Electronic Resource]. — URL: https://rgnkc.ru/zabolevaniya/paroksizmalnaya-takhikardiya.
- Cardiac, or the state of cardiogenic shock. Health and Well-being [Electronic Resource]. — URL: https://www.zdorovieinfo.ru/is_serdechno-sosudistaya_sistema/stati/serdtse_i_sosudy/serdechnyj-ili-kardiogennyj-shok. Interesting article? Share this one with others:

